Discover the key clinical data in AAV
Our current understanding of patient outcomes in ANCA-associated vasculitis (AAV) is rapidly evolving as more studies are being conducted.
Click here to read the key clinical research papers to find out more about treatment outcomes in AAV.
Click here
AAV mechanism of disease
See how the interaction between neutrophils and the alternative complement system are at the heart of the vasculitis process in AAV.
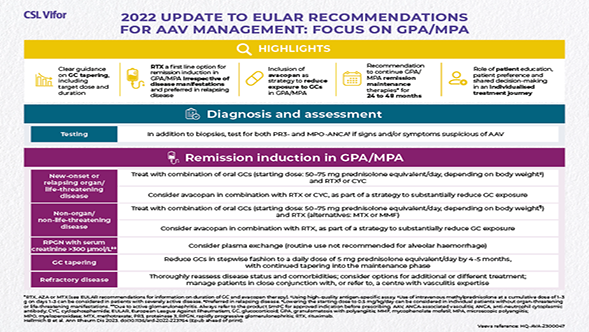
More informationEULAR 2022 recommendations
Download our infographic to view the latest updates and recommendations from EULAR around the treatment of AAV.
DownloadHelpful resources
Use our interactive educational tools to discover more about ANCA-associated vasculitis (AAV).
AAV World is an educational game that sheds light on the clinical priorities in AAV in a fun and interactive way. Take part in AAV World and test your skills through a mix of challenges, brainteasers, riddles and quizzes. Or why not join the Rare Disease Investigation Team and put your expertise to the test in our mysterious challenge.
Complete the challenges
Introduction to AAV
AAV is a rare, severe small vessel vasculitis that affects multiple organs and has a high acute mortality risk1
Read more
Disease Mechanism
The interaction between the activated alternative complement pathway, neutrophils and C5a is at the heart of vasculitic damage in AAV2
Read more